Going Viral
An Uphill Battle
A silent killer lurks in New York City. Virtually invisible when carriers are asymptomatic, the current estimation of respiratory viral infections is largely flawed as it is only comprised of symptomatic data.
The use of vaccines and antiviral drugs have helped prevent the occurrence and spread of some viral diseases, as well as aid in the recovery from infection. However, for many respiratory viral infections (RVIs), excluding influenza, there is no effective means to fight against the viruses especially when infected individuals show no symptoms. The lack of vaccines combined with the high prevalence for recurrence has made RVIs the most common infection among the general population. Additionally, RVIs are the leading cause of hospitalization and mortality in young children worldwide. 1
The current estimation of RVIs is incomplete as it only accounts for symptomatic individuals that seek treatment in medical clinics or emergency departments. In a recent article by Galanti et al., a team aimed to address this shortcoming through the analysis of infection rates among individuals tested regularly for RVIs regardless of their symptoms. They also aimed to elucidate the environmental, demographic, and genetic factors affecting susceptibility, symptomology, and transmission influence on the prevalence of RVIs.
Filling the Viral Void
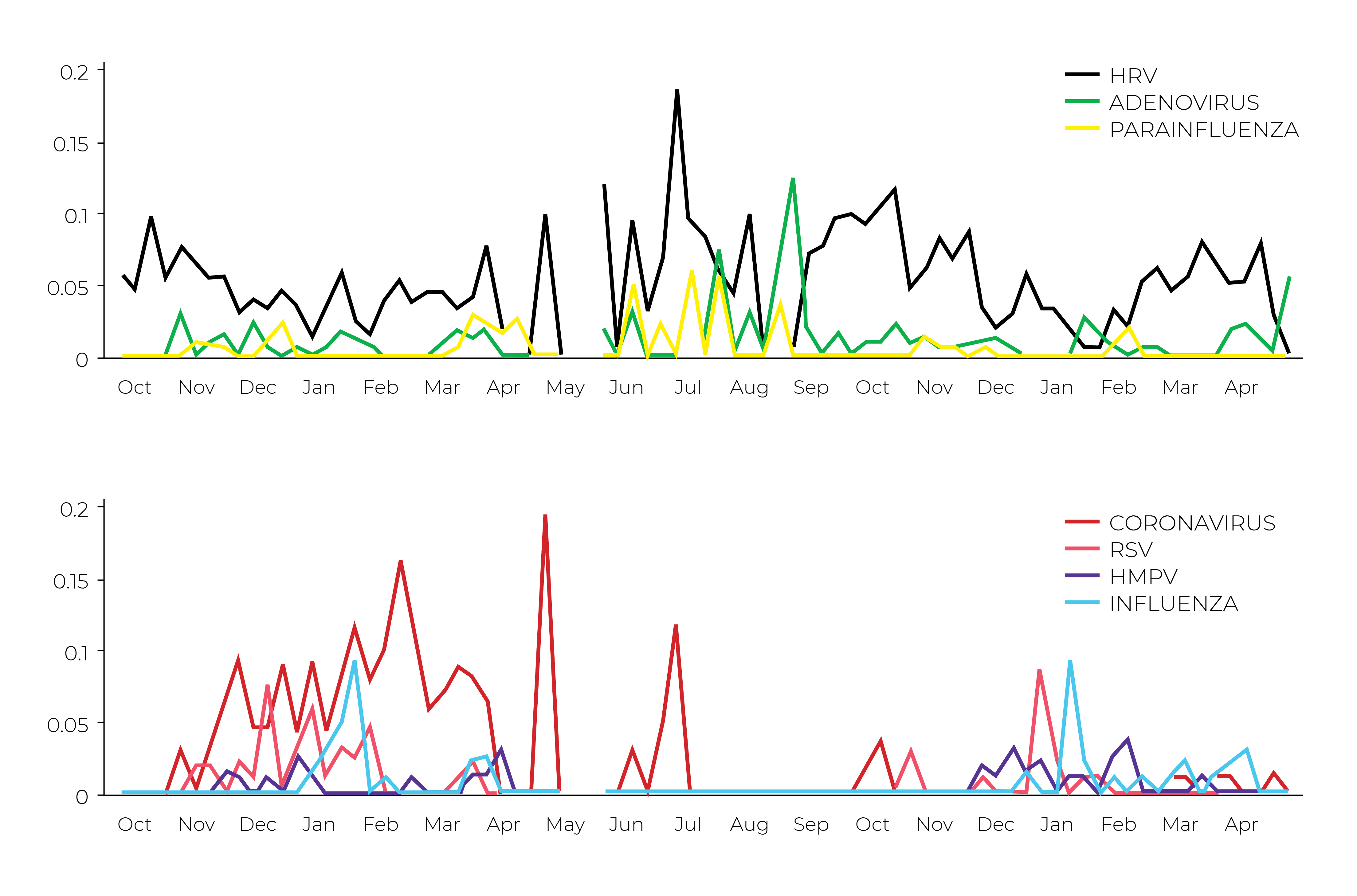
A big void in understanding the epidemiology of viruses is the fact that carriers can be asymptomatic, which is quite problematic. If carriers show no symptoms, how can you correctly diagnose and treat it? This is where longitudinal studies come into play and can fill in the gaps as to who is a carrier and how viruses spread. Galanti et al. enrolled 214 healthy individuals from different locations in the metropolis - New York City, New York. Enrollees consisted of all ages and included adults working in and out of hospital settings, where they may be exposed more to sickly persons. At enrollment, individuals swabbed their both nostrils to provide a baseline survey. Two nasopharyngeal swab samples were collected from each individual weekly according to their enrollment. This was performed for a single cold and flu season (October-April), or the entire study period (October 2016-April 2018), to compare these viruses among different age groups of the population.
To address such a large sample collection process from potentially sick participants, the authors needed to utilize a safe sample collection method compatible with pathogen inactivation and sensitive downstream analysis. Non-invasive nasopharyngeal swab samples from participants were collected using flocked swabs and stored in DNA/RNA Shield at 4-25°C for up to 30 days before long-term storage at -80°C. DNA/RNA Shield was critical in ensuring that any potential viral pathogen was inactivated, while maintaining the integrity of the nucleic acid during collection and storage at uncontrolled temperatures at the site of collection until samples could be brought back to a lab for storage. After storage, nucleic acids were extracted from samples using the NucliSENS® EasyMAG system (bioMerieux), and screened for viruses using the eSensor respiratory viral PCR panel (GenMark Dx).
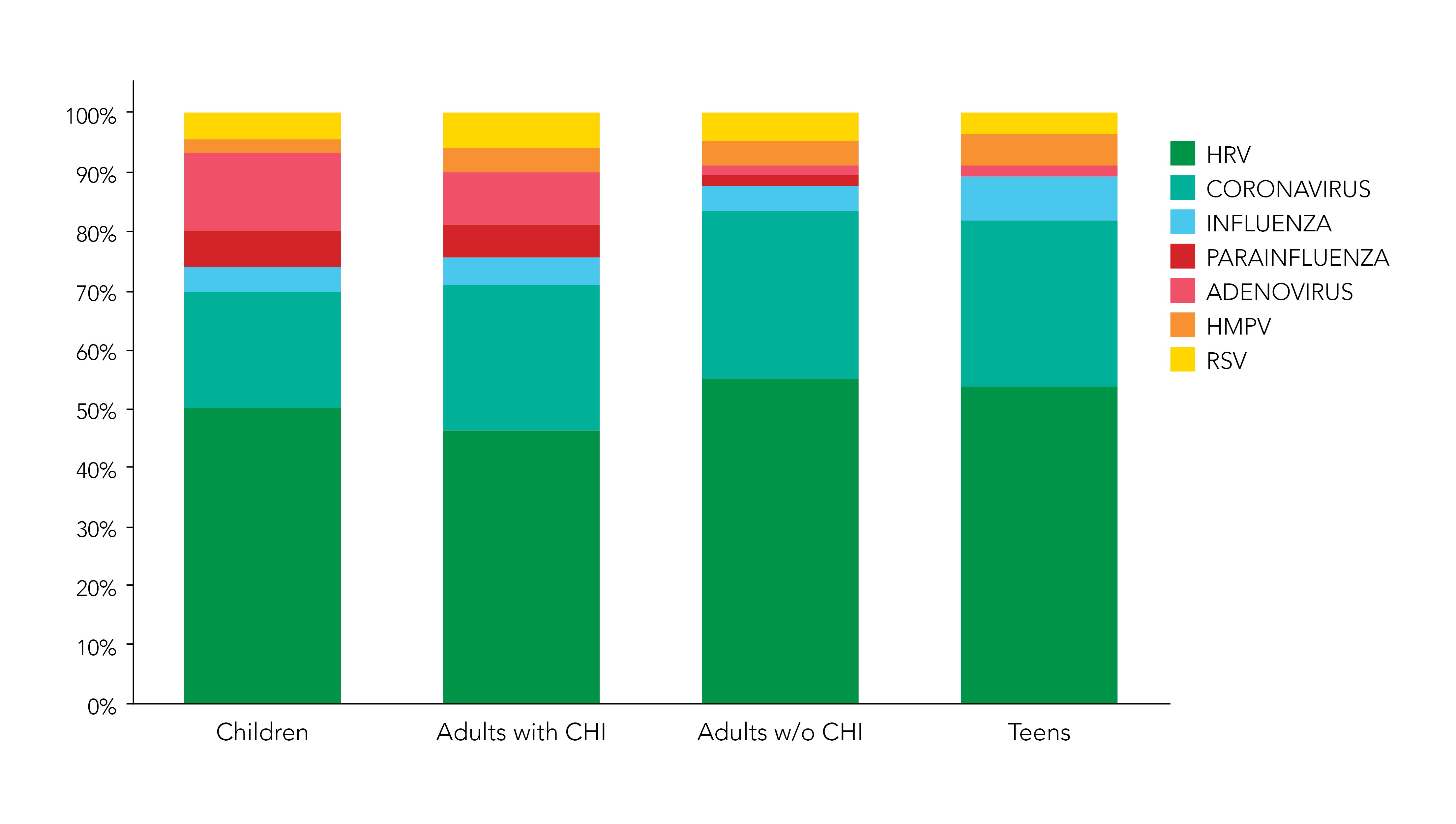
The comparison between children, teenagers, and adults with daily contact with children, and adults without daily contact with children, showed that children presented a significantly higher number of infections than other groups. Interestingly, adults with daily contact with children such as parents and pediatric doctors also showed a higher number of infections than adults without daily contact with children. Furthermore, the distribution of respiratory virus infections for parents and pediatric doctors was very similar to the one in children with higher percentages of adenovirus and parainfluenza than the other groups (Figure 2).
The Conclusion
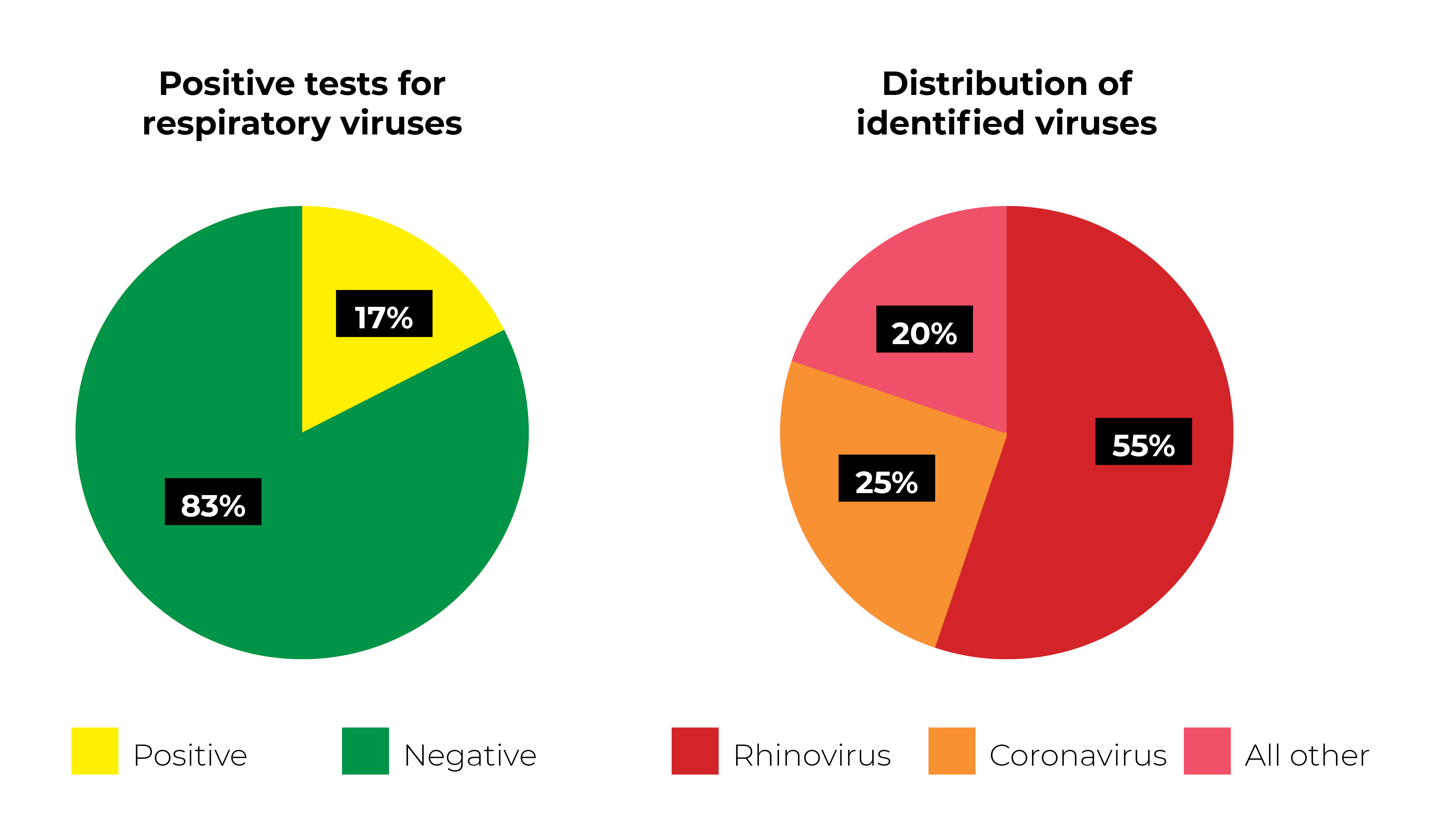
A noticeable difference was observed in results compared to those obtained from traditional syndromic data. According to the study, rhinovirus and coronavirus accounted for over 80% of positive results in all age groups, revealing the contribution of these viruses to the overall infections over the surveillance period. Moreover, they found that respiratory tract infections are strongly connected with age identifying children as the primary source of respiratory tract infection. And subsequently, the parents of these children displayed similar respiratory viral profiles. (Figure 3).
Conducting these types of longitudinal studies can help illuminate the role of asymptomatic transmission of respiratory viruses and provide better data to fully understand what types of intervention are needed to prevent them. They also can help develop epidemiological countermeasures for specific viruses, as well as identify new viruses.
However, the fight against viruses that cause respiratory tract infections is far from over. Researchers are left with a task to find the differences in pathogenicity among these respiratory viruses to get a better understanding about respiratory tract infections.
Surveillance research efforts require high quality DNA and RNA in order to accurately detect viral particles from individuals, which are heavily dependent on optimal sample collection and processing. DNA/RNA Shield is becoming a top choice for viral research for its ability to inactivate pathogens and maintain DNA and RNA integrity for prolonged periods.
For a limited time use code VIRUS25 for a 25% discount on select DNA/RNA Shield products, Quick-RNA Viral Kits, and Quick DNA/RNA Viral Kits (US only).
References:
1. Advani, Sonali, et al. "Detecting respiratory viruses in asymptomatic children." The Pediatric infectious disease journal 31.12 (2012): 1221.
2. Galanti, Marta, et al. "Longitudinal active sampling for respiratory viral infections across age groups." Influenza and other respiratory viruses (2019).
Disclaimer: For direct, domestic U.S. customers only.
*Virus25 promo code is valid for catalog numbers R1100, R1200, R1034, R1035, R1040, R1041, D7020, D7021, R2140, R2141, D7022 and D7023. Offer not valid towards previous purchases. Cannot be combined with any other offer. Void where prohibited by Law or Regulation or Policy. Zymo Researchmay terminate this offer at any time for any reason.


